 An Osteotomy is an operation which changes the alignment of the leg. This can be done for several reasons, though the most common is take pressure of a damaged, or arthritic, part of the knee in order to relieve pain and restore function without resorting to a knee replacement.. It is commonly performed in young, active patients who are developing arthritis in a localised part of the knee and wish to remain active. It is used to relieve pain and to slow the progression of the arthritis, as well as allowing for the resumption of all activites without the restrictions imposed by a knee replacement. Occasionally an osteotomy is used to treat complex knee instability, and in association with cartilage repair or regeneration techniques.
An Osteotomy is an operation which changes the alignment of the leg. This can be done for several reasons, though the most common is take pressure of a damaged, or arthritic, part of the knee in order to relieve pain and restore function without resorting to a knee replacement.. It is commonly performed in young, active patients who are developing arthritis in a localised part of the knee and wish to remain active. It is used to relieve pain and to slow the progression of the arthritis, as well as allowing for the resumption of all activites without the restrictions imposed by a knee replacement. Occasionally an osteotomy is used to treat complex knee instability, and in association with cartilage repair or regeneration techniques.
What is an Osteotomy and how is it performed
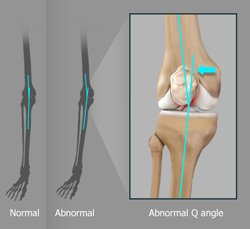
Osteotomy literally means to “cut bone”. After careful preoperative planning one of the bones near the knee (usually the tibia or leg bone, but occasionally the femur or thigh bone) is precisely cut using a small saw to create an incomplete fracture. This cut is then slowly opened to create a wedge, the size of which determines the exact amount of correction. Using infra-red trackers fixed to both bones of the leg, and a receiver connected to a computer, the precise alignment of the entire leg can be measured and fine-tuned during the operation by altering the amount of opening (or size of the wedge). A small plate and screws is then used to hold the bone in place whilst it heals, and in many cases a bone graft is inserted into the created wedge to facilitate this healing process.
Computer aided Navigation
A recent addition to the technique of osteotomy is the use of computer aided navigation. This is the infra-red tracking system mentioned above, and it allows for very precise measurement of alignment whilst the operation is being performed. The alignment can then be carefully adjusted in “real time” and rather than using only measurements calculated before the operation to guide the amount of correction, it allows the surgeon to actually see the alignment change as the osteotomy is being performed. The osteotomy is then only fixed in place when the precise alignment that is needed has been achieved. It also allows the alignment of the leg to be measured not just with the knee fully straight (as traditional techniques do), but throughout its entire range of motion. In this way the osteotomy can be individually tailored to the exact pattern of arthritis of your knee. Prior to the use of this type of intra-operative navigation it was impossible to accurately measure knee alignment in any position except straight. As much knee function occurs on a bent knee the amount of correction in all other positions could only inferred. Using computer aided navigation the alignment throughout the entire knee range of motion can be measured and carefully corrected to get the best result.
Day of surgery and recovery
The operation is generally performed under a general anaesthetic and takes between 60 and 90 minutes. You would be admitted to the hospital on the morning of the surgery and usually spend 1 or 2 nights in the hospital whilst you become accustomed to walking with crutches. Your leg will be placed in a special brace at the conclusion of the surgery which allows controlled movement of the knee whilst supporting the osteotomy. You will wear the brace for 6 weeks, and use the crutches for up to 12 weeks. During the first 6 weeks you take no weight through the leg, and then during the subsequent 6 weeks you gradually increase the amount of weight until you are walking normally. An Xray is taken at the 6 week mark to confirm bone healing before you start to take weight through the leg. A second Xray is taken at the 12 week mark to confirm that the bone has sufficiently healed.
Phyiotherapy
Immediately after the surgery you will be shown some simple exercises to help start the process of rehabilitation, and these can be performed at home. A specific program with a physiotherapist will be commenced 6 weeks after surgery, once sufficient healing has occurred to allow weight bearing. The aim of this program will be to regain the full movement of the knee, and the strength of the muscles around it.
Return to work and sport
Whilst it takes around 6 moths for most patients to fully recover from their osteotomy, it is possible to return to non-physical work around two to four weeks after the operation, as long as this can be done using crutches. For more physical work 3 to 4 months is generally needed before work can be resumed. Sport is recommenced between 6 and 12 months.
Results
High tibial osteotomy generally results in good relief from pain and improvement in function. The majority of patients (over 90%) feel that their knee is much improved after an osteotomy, whilst a small number (5-8%) feel no significant improvement, and 2% feel the knee continue to get worse. The improvement following osteotomy lasts a variable amount of time, though for over 70% of patients the improvement lasts for 10 years or more. There is currently no cure for arthritis and the aim of this operation is not to try to reverse the damage but rather to slow its progression and to improve function by minimising pain.
What happens if the knee gets painful again ?
As discussed above the osteotomy does not reverse the arthritic process within the knee, but rather unloads the damaged part of the knee allowing the more normal parts of the knee to take more of the load. Over time these parts of the knee can also slowly wear out (the most common cause of an osteotomy ceasing to be of benefit is the other parts of the knee developing arthritis). Hopefully this occurs 10 or more after the initially surgery by which time the activity profile of most patients has changed somewhat. When this occurs a total knee replacement can then be performed, with the patient then gaining all the benefits of knee replacement in an arthritic knee. Whilst performing a knee replacement in a patient who has previously had an osteotomy may be slightly more difficult than performing one in a patient who has had no previous surgery, the majority are very successful and it has better results than redoing a previous knee replacement which has worn out and needs redoing.
If it may not last forever why not just perform a knee replacement in the first place ?
Many people ask that if they may eventually need a knee replacement why not just do it in the first place ? This is a good question and some surgeons do take this approach. My reasons for recommending an osteotomy rather than a knee replacement in a suitable patient are the following :
- Osteotomy is generally recommended when the patient is young (generally less than 65). Whilst knee replacements are very effective at relieving pain, they do not last forever. Though over 90% of knee replacements will last more than 10 years these young patients with knee arthritis are going to live a lot longer than that. By performing the osteotomy in these young patients their own, native knee is preserved for longer, and the older the patient is when it finally does come time for the replacement, the more likely the replacement will last the remainder of the patients life
- Osteotomy is recommended when the patient is active. Weather this be their job requirements, or their recreational and sporting activities, if a patient wishes to continue with an active lifestyle an osteotomy may be a better option than a replacement. Knee replacements are very effective at relieving pain and regaining mobility and function that has been lost to arthritis. However they are not designed for vigorous manual labour, or high demand sporting activity. These kind of activities may not be possible after a knee replacement, and even if they are they are not recommended as they will decrease the longevity of the replacement making it more likely that it would wear out sooner and need to be redone. Osteotomy allows for maintenance of a more “normal” knee and the activities that go along with it.
- If the Osteotomy does eventually wear out the option for knee replacement remains. Performing a knee replacement on a patient who has previously had an osteotomy is easier and more effective than redoing a knee replacement which has worn out. An osteotomy does not “burn any bridges” and leaves the option for knee replacement if it should be needed in the future.
In summary an osteotomy “buys time”, allows the patient to remain as active as they wish, and preserves their own native knee for as long as possible. When (and if) the time comes, a knee replacement can still be performed with excellent results, and some patients will never need to progress to a knee replacement.
Risks
All operations have some risk. Those specific include (but are not limited to) :
Incomplete bone healing
In a small percentage (<5%) of patients the bone may not fully heal, or may change position whilst healing. This is monitored by the progress Xray, and in the rare case where it is necessary a second surgery may be required to promote complete healing.
Blood clots
Deep venous thrombosis can occur after any surgery, and is more common after Orthopaedic procedures including osteotomy. All precautions are taken to avoid their occurrence including stockings, calf pumps, and medications. A leg clot which breaks free and travels to the lung can make you very unwell, and in rare cases can be fatal. Any symptom of calf or chest pain, or shortness of breath must be reported to Dr Fritsch immediately. If a blood clot does occur it can generally be treated by medications.
Nerve and blood vessel injury
The major nerves and blood vessels supplying the leg are in the vicinity of the surgery and can rarely be injured. All care is taken to avoid these structures.
Infection
Infection can occur after any surgical procedure. It is uncommon after osteotomy, though possible, and antibiotics are given during the procedure to decrease it risk.
I will discuss the finer points of the risks of surgery with you priot to proceeding. If you have any questions please do not hesitate to ask me until you are satisfied.
Summary
Osteotomy is a very useful technique for preserving function in the young active patient who is developing arthritis. New techniques including the computer aided navigation allow for a high degree of accuracy in tailoring the procedure to an individuals exact disease, and overall this procedure provides excellent results.
